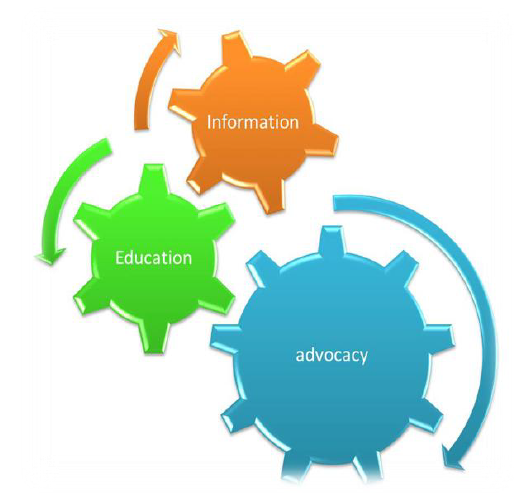
There is a strong link between level of information, education and advocacy and health outcomes in a country.
It has been established through research that most of the diseases can be prevented by imparting accurate and relevant information and education to patients and health care providers. According to the WHO, majority of heart diseases, strokes, Type 2 diabetes and cancer cases could be prevented just by educating and informing people about healthy diet, physical activity/exercise and not using tobacco.
Over one million lives per year could be saved by promoting breast feeding until at least two years and a bulk of under-five deaths could be avoided by educating parents about importance of nutrition and efficient use of their food money which they sometimes spend on sweets for their children to give them as treat.
Globally, adverse drug reactions and irrational use of medicines are among the leading causes of death in many countries. It is estimated that half of all medicines are inappropriately prescribed, dispensed or sold, and that half of all patients fail to take their medicine properly. This problem is particularly serious in developing countries, including many OIC member countries, where less than 40% of patients in the public sector and 30% in the private sector are treated according to clinical guidelines (WHO, May 2010).
The information needs of patients can be met by the pharmacist through participatory education to groups of patients about drug safety, and appropriate use; whereas health workers can be provided with professional training to update their information about diagnose and medication practices.
Like their developing counterparts, many OIC member countries are suffering from the poor level of health information and education.
The situation is particularly critical in low income countries of Asia and Sub-Saharan Africa region. Over the years, immunization campaigns in some member countries have not been effective mainly due to the controversies related with the safety and religious permissibility of the vaccines.
Authorities in member countries like Nigeria and Pakistan have often reported the opposition of religious and political groups to carry out national polio vaccination campaigns. To overcome this problem, the OIC GS secured a religious injunction from the Islamic Fiqh Academy which issued a fatwa to encourage the Muslims to participate and support the national polio vaccination campaigns.
Quoting extensively from the Qur’an, the fatwa lays out the duty to protect children when disease is preventable. Thus, the fatwa addresses the critical need to raise awareness in Muslim communities about the benefits of polio immunization campaigns.
However, there is a strong need for similar fatwas to support all kinds of immunization campaigns in OIC member countries.
In general, family planning related measures have also been less effective mainly due to the lack of information and education of health workers as well as the target groups. Based on the research conducted by various national and international health agencies, lack of knowledge, access problems and side-effect fears were the major limiting factors for the use of family planning measures in many OIC member countries.
Not only a majority of population generally lacks the basic knowledge about these measures but also many have misleading information. For example, many people believe that use of contraceptives is not permissible in Islam, whereas others believe that it is unhealthy and can affect the fertility and hence those who are using contraceptives will not be able to bear children later on.
The problems related with lack of knowledge and access could be addressed by increasing the community-wide awareness about the family planning especially through the involvement of local religious leaders and ensuring the availability of contraceptives in a locality. The community awareness campaigns should particular focus on the contraceptive usage to help address negative perceptions about it.
Another major challenge in OIC member countries is the information and education deficiencies of health workers. Like their counter parts in many other developing countries, health care providers in OIC member countries continued to lack basic, practical information and expertise to enable them to deliver safe and effective health care.
This lack of knowledge about the basics on how to diagnose and manage common diseases, lead to ineffective and dangerous health care practices which are resulting into the failure of even the most modern medicines and causing many avoidable deaths. Irrespective of the level of economic development and progress, according to the findings of some investigative studies (Neil & Frederick, 2009), there is a considerable knowledge and awareness gap both among health care providers and patients in many OIC member countries.
The challenges in the area of medical and nursing education are more or less common to all OIC member countries. Despite progress made in updating medical and nursing curricula in selected institutions, the majority of schools still follow traditional programmes which, by and large, have not evolved to become competency-based. Family medicine training programmes have been initiated in several countries, however their scope remains limited.
Underlying factors in the lack of progress in this area include: the lack of effective coordination between service providers including ministries of health and higher education institutions, the limited institutional capacity to provide large-scale training for family physicians, as well as for converting the existing cadre general practitioners to family physicians through customized programmes; and the inability to establish family medicine as an attractive career path for fresh graduates.
The key challenges to ensuring access to quality nursing education in the OIC countries pertain to inadequate investment and low priority given to nursing education; lack of capacity in nursing schools in terms of the availability of trainers as well as infrastructure; the need to further update nursing curricula in order to bridge the service-education gap; the limited institutional capacity to offer post-basic training programmes; and inadequate emphasis on continuous professional development programme.

